
Stacy B. Menees1,2*, Jason R. Baker1, Kenya Jackson3, Tanvi Goyal4, William D. Chey1
*1Division of Gastroenterology, Michigan Medicine, Ann Arbor, MI.
2Division of Gastroenterology, Department of Internal Medicine, Ann Arbor Veterans Affairs Medical Center, Ann Arbor, MI.
3Trauma Services, Grady Memorial Hospital, Atlanta, GA.
4Department of Internal Medicine, Michigan Medicine, Ann Arbor, MI.
*Corresponding author: Stacy B. Menees, Division of Gastroenterology, Michigan Medicine, Ann Arbor, MI.
Received date: February 15, 2023
Accepted date: May 20, 2023
published date: June 28, 2023
Citation: Stacy B. Menees, Jason R. Baker, Kenya Jackson, Tanvi Goyal, William D. Chey. (2023) “The Effect of Bariatric Surgery on Obesity–Related Hypersomnolence: A Literature Review”, J of Gastroenterology and Hepatology Research, 4(1); DOI: http;//doi.org/02.2023/2.10137.
Copyright: © 2023 Stacy B. Menees. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly Cited.
Background: The aim of this study was to assess for gender differences in fecal incontinence (FI) severity, quality of life, and anorectal function & sensation.
Methods:
A retrospective analysis of patients with FI who underwent high resolution anorectal manometry (HRARM) at a tertiary care center was performed. At the time of ARM, patients completed two validated surveys: the Fecal Incontinence Quality of Life Instrument (FIQL) and Fecal Incontinence Severity Index (FISI). HRARM characteristics included: high pressure zone (HPZ), resting and maximum squeeze pressures, rectal sensation (first sensation, urgency, maximum tolerated. Bivariate analyses with student’s t test and Pearson’s chi square test were performed to assess the association between gender and HRARM/FISI/FIQL.
Key Results: 336 consecutive patients with FI underwent HRARM. FI severity did not differ between genders (36.2+12.8 vs. 33.8+15.6, p=.22). FIQL subscales showed a difference in coping/behavior subscale, with women reporting more difficulty than men (1.95 vs. 2.25, p=.004). HRARM values significantly varied by gender with women having a shorter high-pressure zone, lower resting pressures, decreased squeeze and lower maximum tolerated volume. For rectal sensation, only maximum tolerated volume differed between women and men.
Conclusions & Inferences:
Though overall FI symptom severity is similar between women and men; women have more difficulty coping with FI than men. HRARM and rectal sensory testing identified gender-based differences which could put women at greater risk for urge-related FI.
Introduction:
Fecal incontinence (FI), as defined as the unintentional loss of liquid or solid stool, is a common disorder affecting up to 14.4% in population-based studies.[1-3] Recently, a large population-based study of FI patients utilizing the National Institutes of Health (NIH) FI Patient Reported Outcomes Measurement Information System (PROMIS) questionnaire found gender differences in the clinical presentation of FI. [3] Men were less likely to have urge-associated FI (OR .71, 95% CI .63-.79, women were reference group), but were more likely to have accidental loss when they thought they were passing flatus (1.29, 1.16-1.43). Prior to this study, few differences have been demonstrated between men and women who have fecal incontinence.
Anorectal manometry (ARM) is a useful tool to assess the neuromuscular function of the rectum and anal canal. Recently, high resolution anorectal manometry (HRARM) has been developed and shown to provide more useful physiological assessment of anorectal function. With the aforementioned findings, we hypothesized the following utilizing HRARM: women are likely to show a greater deficit in the squeeze pressure than men; and men are more likely to have abnormal sensation as compared to women (i.e., decreased sensation, higher sensory thresholds). Therefore, the aim of this study is to assess for gender differences in FI severity, impact of quality of life, and anorectal function & sensation which might account for the clinical differences reported by women and men.
Materials and methods:
Study Design:
This study is a retrospective analysis of patients with the diagnosis of FI who underwent high resolution anorectal manometry at a tertiary care center. Institutional Review Board approval was attained through the University of Michigan prior to initiation of the study. At the time of HRARM, patients who had the diagnosis of FI, completed a demographics questionnaire and two validated surveys: the Fecal Incontinence Quality of Life Instrument (FIQ-L) and Fecal Incontinence Severity Index (FISI). The FIQ-L is a validated questionnaire assessing health-related QOL to address issues related specifically to FI which is composed of 29 items that compile four subscales including lifestyle, coping behavior, depression/self-perception and embarrassment. [4] The score range is 0-5 with a higher score indicating better QOL or being less affected. The FISI is a tool to assess severity of FI with a score range of 0-61 with higher scores reflective of worse FI severity. [5] HRARM characteristics that were collected included the following: high pressure zone (HPZ), resting and maximum squeeze pressures, rectal sensation (first sensation, urgency, and maximum tolerated). Only patients with the indication of FI for the HRARM were included in the study. Any subject with any other indication listed for the HRARM was excluded.
HRARM Procedure:
For the procedure, an enema is given if stool is detected on digital rectal examination. At least thirty minutes elapse from enema insertion to the start of the procedure. Patients are placed in the left lateral position with knees and hips bent at a 90° angle. The lubricated Sandhill high-resolution anorectal manometry probe (Sandhill Scientific, Denver, CO, USA) is inserted into the rectum. Data are obtained on rest, squeeze, cough reflex, simulated defecation, graded balloon distension (threshold, urgency and maximal tolerated). Data are analyzed using the Bioview analysis software with the InSIGHT G3 HRiM or InSIGHT Ultima system (Sandhill Scientific).
Statistical Analysis:
Descriptive statistics of the FI cohort were used to describe demographics and baseline symptoms. Our primary outcome was to assess gender differences in HRARM measurements. Our secondary outcomes assessed for gender differences in FISI and FIQL questionnaires. Bivariate analyses with student’s t test and Pearson’s chi square test were used to assess for gender differences in FISI questionnaire scores, the four FIQL domain scores and HARM findings. Covariates included demographics age, race, BMI, gender, diabetes mellitus, history of hemorrhoidectomy, spine surgery, urinary incontinence, irritable bowel syndrome (IBS) and obstetric history (episiotomy, caesarian section, vaginal delivery. Based on the bivariate analysis of the HRARM findings, each subject’s HRARM findings were dichotomized into low vs. normal or high, based on established test parameters for each gender. [6] All associations with a p value of .10 or less were included in each HRAM model. Saturated multivariable logistic regression models were used to determine independent predictors for each positive HRARM finding. Additionally, an analysis to assess for gender differences in the type of FI experience was also performed. Each of the FISI categories (gas, mucus, liquid stool or solid stool) were dichotomized into either “any FI episode of that category” or no FI. Data analyses were conducted using SAS 9.4 (SAS Institute Inc. Cary, NC) with significance set at an alpha of 0.05.
Results:
Demographic Data:
Between 06/01/2015 and 10/01/2017, a convenience sample of 1368 outpatient HRARM were performed. After applying inclusion and exclusion criteria, 336 patients were available for analysis. 73.5% were female and 88% were Caucasian with a mean age of 60.9 (+14.8). Mean BMI was 28.4 (+6.1). Comorbidities reported included IBS (34.7%) and diabetes mellitus (19.9%). Demographics by gender are detailed in Table 1. Women were more likely to report IBS (p<.0001) and urinary incontinence (p=.02) compared to men. Men were more likely to report tobacco use as compared to women (p=.02).
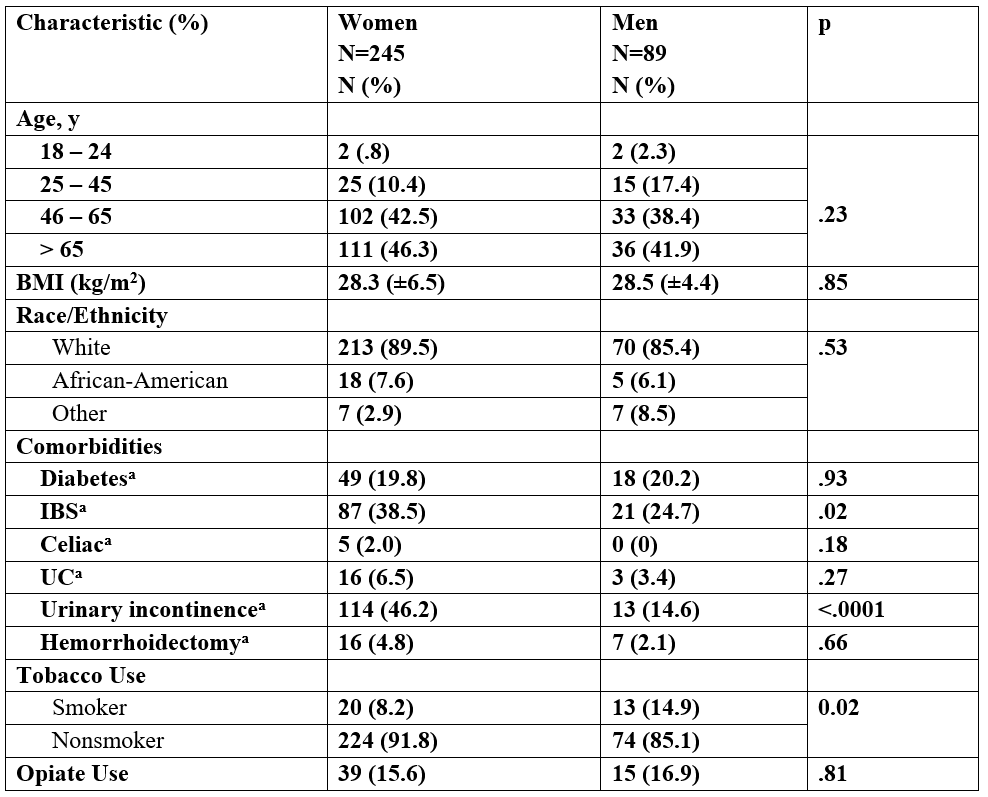
a Physician-reported diagnosis
Table 1: Patient Demographics
FISI and FIQL questionnaires:
Mean FISI was 35.6 (+13.6) with mean FIQL subscales: lifestyle 2.72 (+.92), coping behavior 2.03 (+.8), depression/self-perception 2.55(+.76), embarrassment 2.03(+.8). Severity of FI did not significantly differ between women vs men (36.2+12.8 vs. 33.8+15.6, p=.22). (Table 2) However, women were much more likely to experience solid stool incontinence compared to men (OR 1.97, 95% CI 1.1-3.5) but there was no difference in either gas or liquid stool incontinence. (Table 3) FIQL subscales showed a difference in coping/behavior subscale, with women reporting more difficulty than men (1.95 vs. 2.25, p=.004). (Table 2)
|
Fecal Incontinence Symptoms or Related Outcomes |
|
Women |
|
Men |
|
P valuea |
|
Fecal Incontinence Severity Index (mean ± SD) |
|
36.2 ± 12.8 |
|
33.8 ± 15.6 |
|
.22 |
|
FIQL (mean ± SD) |
|
|
|
|
|
|
|
Lifestyle |
|
2.69 ± .91 |
|
2.81 ± .94 |
|
.29 |
|
Coping/Behavior |
|
1.95 ± .76 |
|
2.25 ± .84 |
|
.004 |
|
Depression/Self Perception |
|
2.54 ± .75 |
|
2.54 ± .75 |
|
.97 |
|
Embarrassment |
|
1.99 ± .82 |
|
2.15 ± .81 |
|
.17 |
a Based on Paired Student’s t test
Table 2: FISI and FIQL Questionnaires by Gender
|
Type of Incontinence |
|
Women N=245 N (%) |
|
Men N=89 N (%) |
|
OR (95% CI) |
|
|
Solid |
|
155 (63) |
|
46 (49) |
|
1.97 (1.1-3.5) |
|
|
|
|
|
|
|
|
|
|
|
Liquid |
|
182 (74) |
|
62 (69) |
|
1.82 (.86-3.84) |
|
|
|
|
|
|
|
|
|
|
|
Gas |
|
189 (77) |
|
68 (76) |
|
2.22 (.84-5.87) |
|
|
|
|
|
|
|
|
|
|
|
Mucus |
|
118 (48) |
|
45 (50) |
|
.79 (.45-1.41) |
|
˟ Reference Group
Table 3: Incontinence Type by Gender
HRARM results:
HRARM values significantly varied by gender with women having lower resting pressures (p<.0001), decreased squeeze (p<.0001) and a shorter high pressure zone (p<.0001). (Table 4) For rectal sensation, only maximum tolerated volume differed between women and men (p<.0001). These findings are confirmed on multivariable logistic regression (Supplementary Tables 1-5). With multivariable logistic regression for all HRARM components that were positive on bivariate analysis, we found additional associations (supplementary tables 1-5). The model for low resting pressure demonstrated a small but significant effect of age (OR 1.03, 95% CI 1.01-1.05) and BMI (OR .96, 95% CI .92-.99). Women had a 2.38 higher odds (95% CI 1.29-4.27) of having low resting pressure than men. The final model for low squeeze pressure demonstrated age (OR 1.03, 1.01-1.04), women (OR 2.47, 95% CI 1.43-4.25), and episiotomy (OR 8.0, 95% CI 1.03-62.2) as significant contributors. For the short high pressure zone model, only female gender (OR 2.26, 95% CI 1.36-3.83) was a positive predictor. Lastly, the final model for predictors of a low maximal tolerated volume demonstrated that female gender (OR 2.24, 95% CI 1.3-3.8) and Caucasian race (OR 2.77, 95% CI 1.3-6.1) had a higher likelihood of a low maximal tolerated volume as compared to men.
|
HRARM Measures |
|
Women |
|
Men |
|
P value |
|
High pressure zone (cm) |
|
3.43 |
|
4.04 |
|
<.0001 |
|
Resting pressure (mmHg) |
|
52.36 |
|
68.26 |
|
<.0001 |
|
Maximum Squeeze (mmHg) |
|
114.1 |
|
189.1 |
|
<.0001 |
|
First Sensation (ml) |
|
56.86 |
|
54.15 |
|
.50 |
|
Urgency (ml) |
|
93.09 |
|
101.8 |
|
.10 |
|
Maximum tolerated (ml) |
|
127.9 |
|
157.4 |
|
<.0001 |
Table 4: High Resolution Anorectal Manometry by Gender
Post Hoc Statistical Power Analysis:
A post hoc power analysis was conducted using the 2-sample means proc power procedure in the software package SAS 9.4 (by SAS Institute Inc., Cary, NC, USA). The sample size of 336 was used for the statistical power analyses. The alpha level used for this analysis was p < .05. The post hoc analyses revealed the statistical power for this study to test gender differences for 4 HRARM characteristics: high pressure zone, resting pressure, maximum squeeze and maximum tolerated. The power exceeded .99 for the detection of the observed effect sizes for all 4 of the between-group characteristic comparisons.
Discussion:
This is one of the largest HRARM study in FI patients and is the first to specifically look for differences between women and men. The HRARM and rectal sensory testing identified gender-based differences which could put women at greater risk for urge-related FI. These findings were robust even after controlling for potential confounding factors. Although overall FI symptom severity is similar between women and men, women are more likely to report solid stool incontinence and have more difficulty coping with FI than men.
Despite accounting for known gender differences in HRARM and other demographic factors, women in our study were more likely to have low resting pressure, low squeeze pressure, shorter high-pressure zone and a lower maximum tolerated rectal volume as compared to men. Women are different from men when it comes to FI. Our HRARM findings support a higher likelihood of urge incontinence in women as we initially hypothesized. These results are consistent with results from a large population based survey of people from the US with FI. [3] We also found a female-specific association with episiotomy increasing the likelihood for low squeeze pressure. Manometric differences among women with a history of episiotomy was first reported by Perry and colleagues.[7] The authors reported a low mean vector symmetry index in six women with only a history of episiotomy. In a German study, Franz et al. found reduced squeeze pressure in women with midline episiotomy assessed at a median of 21 weeks postpartum.[8] Fortunately, obstetric practices are changing, with guidelines recommending against routine episiotomy with vaginal delivery, thus practitioners should see less of this in the future. However, this call for a change in practice only began in 2005 where a systematic review by Hartmann et al. found no benefits to routine episiotomy.[9] In 2006, the American Congress of Obstetricians and Gynecologists issued new guidelines, stating that episiotomy during labor should be restricted.[10]
For both resting and squeeze pressure measurements on HRARM, we found additional associations besides gender. Increasing age was associated with both low resting pressure and low squeeze pressure. Our findings are congruent with prior studies on the impact of age on the internal anal sphincter.[11-13] With age, the internal anal sphincter thickens due to probable fibrosis which then generates less resting pressure compared to active muscle fibers.[13] For the external anal sphincter, the impact of age on its functioning is less clear. Studies have found either no impact [13-16] or a reduction in squeeze pressures with aging.[11, 17] We found a 3% higher likelihood of squeeze reduction with every year increase. For resting pressure, we also found that increasing BMI was protective against low resting pressure on HRARM. This finding has been described previously [6, 18] but seems counterintuitive as obesity is a risk factor for FI. [19-21] One possible explanation is that obesity induces a higher abdominal pressure and requires recruitment of more muscle fibers to maintain the resting pressure. [6] This then leaves less motor fibers available to recruit for episodes of leakage and suggests a decreased threshold for leakage in obese individuals. Similarly, this has been seen in the urinary incontinence (UI) literature, where obese women with UI, have normal to high resting urinary sphincter pressure. [22-24]
We did not find evidence for abnormal sensation in men that could account for an increased risk for accidental FI. Men were twice as likely to have a lower threshold sensation as compared to women (21.6% vs. 9.84%) which could be seen as protective against FI. However, an elevated threshold sensation volume increases the likelihood of FI was seen equally in men and women (20.5% vs. 20.1%). For urge sensation, there was no significant difference by gender, although the men in our cohort reported a slightly lower percentage of normal urge sensation as compared to women (31.4% vs. 37.8%) but this was not statistically significant. Having decreased rectal capacity with a lower maximum tolerated volume was also more likely to be seen in women rather than men. The women in our cohort had a 2.2-fold higher likelihood of this finding compared to men. This may suggest a component of reduced rectal capacity as contributor to the pathophysiology of FI in our female cohort. Disordered sensation, both hypo- and hypersensitivity has been reported in the literature as an important contributor to FI symptomotology. [25-29]
A strength of this study is that is one of the largest series of HRARM studies in patients with FI. However, there are several limitations. Despite this being a retrospective analysis, the data was prospectively collected, and we utilized validated questionnaires. Retrospective analysis provides a challenge to control for the environment of this sensitive and intimate diagnostic test. However, all high-resolution anorectal manometry tests were performed by only three specially trained gastro-intestinal physiology technicians, utilizing the same catheter design, identical testing protocols, and interpreted by only one provider. The cross-sectional study design may introduce bias for FIQOL and FISI measurements since these measurements were collected prior to anorectal manometry testing without controlling for anxiety metrics.
In summary, HRARM and rectal sensory testing identified gender-based differences which could put women at greater risk for urge-related FI. Episiotomy was a contributor to those gender-based differences, which will continue to occur less frequently in the future based on guideline recommendations. Additionally, our study did not find significant differences in rectal sensation between women and men that could account for a higher likelihood of accidental FI. Future studies with rectal barostat or EndoFLIP to assess rectal compliance could be used to help further elucidate possible differences between women and men.
Supplementary Tables:
|
Characteristics |
OR (95% CI) |
|
Age |
1.022 (1.004-1.041) |
|
Sex |
2.384 (1.241-4.578) |
|
BMI |
0.960 (0.920-1.001) |
|
Diabetes |
1.743 (0.905-3.357) |
|
Caucasian |
0.890 (0.410-1.933) |
|
Episiotomy |
8.158 (1.030-64.639) |
|
Vaginal Deliveries |
0.936 (0.777-1.128) |
|
UI |
2.043 (1.184-3.527) |
Table 1: Multivariable Logistic Regression (OR [95%/CIs]) Estimates of Predictors of low squeeze pressure on ARM(Anorectal Manometry)
|
Characteristics |
OR (95% CI) |
|
Age |
1.033 (1.015-1.052) |
|
Sex |
2.197 (1.207-4.000) |
|
BMI |
0.958 (0.920-0.998) |
|
Caucasian |
0.543 (0.254-1.159) |
|
Episiotomy |
1.823 (0.644-5.156) |
Table 2: Multivariable Logistic Regression (OR [95%/CIs]) Estimates of Predictors of low resting pressure on ARM (Anorectal Manometry)
|
Characteristics |
OR (95% CI) |
|
Age |
0.999 (0.983-1.016) |
|
Sex |
2.262 (1.336-3.831) |
|
BMI |
0.967 (0.930-1.005) |
|
Diabetes |
0.699 (0.390-1.252) |
|
Caucasian |
1.212 (0.589-2.497) |
Table 3: Multivariable Logistic Regression (OR [95%/CIs]) Estimates of Predictors of high pressure zone on ARM (Anorectal Manometry)
|
Characteristics |
OR (95% CI) |
|
Age |
0.997 (0.981-1.014) |
|
Sex |
2.238 (1.303-3.843) |
|
BMI |
0.989 (0.950-1.028) |
|
Diabetes |
1.743 (0.905-3.357) |
|
Caucasian |
2.769 (1.266-6.058) |
Table 4: Multivariable Logistic Regression (OR [95%/CIs]) Estimates of Predictors of low maximal tolerated on ARM (Anorectal Manometry)
|
Characteristics |
OR (95% CI) |
|
Age |
1.011 (0.987-1.034) |
|
Sex |
0.408 (0.175-0.951) |
|
BMI |
1.014 (0.956-1.075) |
|
Diabetes |
1.142 (0.504-2.584) |
|
Caucasian |
>999.999 (<0.001->999.999) |
|
Vaginal Deliveries |
0.936 (0.777-1.128) |
Table 5: Multivariable Logistic Regression (OR [95%/CIs]) Estimates of Predictors of low threshold on ARM (Anorectal Manometry)
Grant Support: This study was unfunded.
Abbreviations: FI fecal incontinence, DM diabetes mellitus, GI gastrointestinal, IBS irritable bowel syndrome, NIH National Institutes of Health, PROMIS Patient Reported Outcomes Measurement Information System
Disclosures: Dr. Chey is a consultant for Allergan, Biomerica, IM Health, Ironwood, Outpost, QOL Medical, Salix, Shire, and Urovant and research grants from Biomerica, Commonwealth Diagnostics, Nestle, QOL Medical, and Zespri. Dr. Chey are also patent holders and principals at My Total Health. Dr. Baker, Dr. Goyal and Kenya Jackson do not have any disclosures.
Writing Assistance: None.
Author Contributions: